Eye Surgeon's Surgical Notes: Trabeculectomy
- Atanas Bogoev M.D.

- 6 hours ago
- 5 min read
A Glaucoma Surgery Guide by Atanas Bogoev, MD, FEBO, a glaucoma and anterior segment surgeon, working in University Hospital Bochum, Germany.
This surgical note summary is my personal one, and it was inspired by The Moorfields Safer Surgery System for filtering glaucoma surgery, as well as my personal learning experience at University Hospital Bochum. Special credits to Prof. B. Dick for the mentorship and Dr. Devesh Varma's method of surgical education, which I learned during my observership in Toronto, Canada.
1. Choosing the correct site
The Moorfields Safer Surgery System provided us with one of the most fundamental insights: cystic blebs with limited posterior flow create the “ring of steel” (a ring of steel is intense scar tissue around a post-operative bleb, caused by restricted posterior aqueous humor drainage), a hallmark of failure.
Every maneuver, instrument, and tissue handling is designed to promote diffuse posterior flow, minimize scarring, and enhance safety and predictability.

The preferred surgery site:
Superior hemisphere (superonasal or superotemporal): Lower inflammation, better bleb protection from the lid, and fewer complications like dysesthesia (foreign body sensation) and recurrent hemorrhages.
Avoid Inferior Sites unless no superior tissue remains; consider using a tube instead.
2. Traction Suture
Instrument: 6-0 or 7-0 black silk on a semi-circular needle
Location: Superior peripheral cornea
Why this matters:
Avoids superior rectus trauma, bulbus perforation, or hematoma.
Provides an optimal superior vector of traction.
If placed at the correct lamellar depth, there is a relatively low risk of “cheese-wiring” or ocular penetration
In a retrospective comparative study of 385 eyes at the Second People’s Hospital of Jinan (206 eyes with superior rectus traction suture vs. 179 with peripheral lamellar corneal traction suture), after 24 months of follow-up, trabeculectomy using the corneal traction suture had a higher qualified success rate (94.4% vs. 88.3%), more diffuse blebs, less bleb vascularity, and fewer encysted blebs than the superior rectus traction suture.
Li B, Zhang M, Liu W, Wang J. Comparison of Superior Rectus and Peripheral Lamellar Corneal Traction Suture during Trabeculectomy. Curr Eye Res. 2016;41(2):215-21. doi: 10.3109/02713683.2015.1009635. Epub 2015 Sep 15. PMID: 25803293.
3. Conjunctival Incision
Limbal Incision with targeted length: 7-10 mm (1.5 to 2 clock hours) - I make it just wider than my planned scleral flap size.
Instruments: Limbal cut with 15-degree Blade / blunt dissection with Westcott Scissors

No relaxing incisions. This reduces wound trauma and improves postoperative wound integrity.
Less technically demanding.
More conducive to posterior aqueous flow and diffuse bleb formation.
4. Scleral Flap Creation
Shape: Rectangular
Sequence:
Measuring with a caliper 3.5 mm wide and 2 mm long, measuring from the blue zone
Marking (you can mark bluntly with your caliper or use dyes)
Horizontal incision parallel to limbus
Lamellar dissection forward into clear cornea
Side incisions (not up to limbus to encourage posterior flow)
Flap must be:
Large enough to resist uncontrolled flow
Thick enough to avoid cheese-wiring - ideally 50% scleral thickness
Avoid large aqueous veins (bleed, increased scaring risk)
READ MORE: Limbal Landmark Anatomy by Insight Ophthalmology

5. Conjunctival Pocket Creation
Conjunctival Dissection:
Use blunt dissection with Westcott scissors to create a wide posterior pocket under the conjunctiva and Tenon’s.
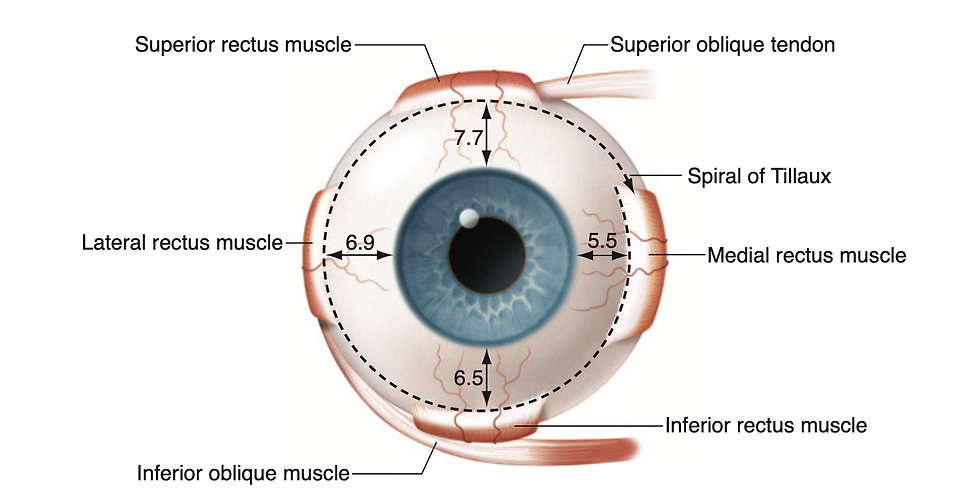
Carefully dissect over the superior rectus muscle - dissect bluntly superior laterally and superior nasally and try to stay away from the 12 o'clock position, where we expect the muscle. Remember the Spiral of Tillaux - we expect the superior rectus about 7.7 mm from the limbus.

Timing of Antimetabolites:
Apply after scleral flap creation but before entering the eye. We do not want them to enter intraocularly.
Antimetabolites:
If using Mitomicine: 0.2–0.5 mg/mL × 3 minutes (we use 0.3 mg/mL for 3 min)
If you do not have access to MMC you can using 5-Fluorouracil (5-FU): 50 mg/mL for 3 minutes
Avoid antimetabolite contact with the surface of the conjunctiva, cornea or limbus.
Rinse thoroughly with ≥20 mL BSS
Treat a diffuse area posteriorly and laterally to prevent a “ring of scar”.
6. Mitomicyn Strategy and Sponge Insertion
Circular non-fragmenting polyvinyl alcohol (LASIK-type) sponges are inserted into the pocket without touching the conjunctival edge. Keep it away from the limbus - this avoids complications like avascularity at the limbal area.
Aim to maximize surface contact, minimize wound trauma and leakage risk.
Count the number of sponges you insert and remove!
7. Paracentesis
Paracentesis:
The oblique tunnel parallel to the limbus directed towards
Lateral or lateral-inferior placement allows access for aqueous taps or anterior chamber reformation.

8. Sclerostomy
Instruments:
Kelly Descemet's Membrane Punch (0.75 mm) or
Corneal Trepan (1.0 -1.5 mm)
Manual trepanation (targeting 1.0 - 1.5 mm scerostomy)
Aim at the perpendicular at the sclerolimbal junction, targeting the anterior trabecular meshwork.
Decement Membrane Punches or trepanes give you the advantage of :
Less trauma
Predictable outflow
Smaller wound with less astigmatism, less flow turbulence
Try to use precision instruments if they are available.
9. Peripheral Iridectomy

Target: Prevent iris occlusion or pupillary block
Start with lifting the scleral flap with Colibri.
Use thin iris forceps with teeth to grab the iris base and pull so that you have about 0,5 mm of iris visible through the wound.
Use scissors parallel to limbus to create a small, wide, controlled iridectomy
Use BSS to flush the Iris Pigment layer and confirm a patent Iridectomy.
Do not:
Enter or manipulate with the vanas scisors intraocularly
Do not flush profusely with BSS. You can get Iris prolapse through the sclerostomy.
10. Scleral Flap Sutures

Suture Material: 10-0 monofilament nylon
(Optional) Pre-place 2 corner sutures while the eye is still firm (before performing the sclerostomy)
Tie the posterior corner sutures first
Check for leakage and put more suture if needed.
Use the slip knot so that you can adjust the tension later.
Assess flow: via BSS inflation of the anterior chamber.
Adjust suture tension so that you have a brisk flow with the desired IOP. Take care to observe the anterior chamber depth.
Post-op Adjustability:
Releasable or transconjunctival adjustable sutures
Instruments: Flat-tipped Adjustable Suture Forceps
Laser Suturolysis

11. Conjunctival Closure
Suture: Continuous limbo-conjunctival 10-0 nylon.
This prevents central retraction, leakage, and discomfort.
Final Test: Inject BSS in the AC - confirm no conjunctival leakage

Postoperative management is as important as the surgery itself. Control strictly and intervene early to avoid complications.
Additional resources:
Ike Ahmed's Trabeculectomy Technique with Mitomycin-C
Surgery: Trabeculectomy: Dr. James Brandt (Orbis)

Eye Wiki's Comprehensive Trabeculectomy Article - one of the most comprehensive resources, including diagnostics, indications, contraindications, and complications.

Conclusion
Using the Moorfields Safer Surgery System and adapting it to your current setting is the best protocol to follow. At the end, you want to have controlled aqueous flow, minimal trauma, and maximal posterior filtration.
Every move during the surgery should be intentional, evidence-based, and flow-optimizing. With this system, the safety and efficacy of trabeculectomy can be improved and extended. I hope you are inspired by my notes and develop your own, and try to add individualised additions on each step that you need. Good luck!
ABOUT THE AUTHOR
Atanas Bogoev, M.D., FEBO is a consultant ophthalmologist, eye surgeon, and co-founder of Ophthalmology24. Atanas has trained internationally, attending courses at Harvard Medical School, Oftalmo University, and completing observerships such as the GAASS program in Toronto. He combines surgical experience with a passion for education, translating surgical best practices and clinical learning into accessible resources.









